|
In additional to classroom lectures and practical skill building exercises, EMT students are required to complete 10 hours of practical experience outside the classroom. For most students, this means time in the Emergency Department (ED) of a local hospital. Thanks in part to the fact that my EMT course is being taught through Atlantic Health's training arm, I was lucky enough to swing a shift with our local paramedics from the Mobile Intensive Care Unit or MICU.
Paramedics are an absolutely critical part of the EMS community. While EMTs have basic life support skills that are more than sufficient for many situations, Paramedics bring options for a higher level of care, especially when it comes to pharmacological options such as providing pain and other medications (often intravenously). They also provide advanced airway management options, such as intubation, that EMTs are not qualified to perform directly.
Of course, it's also useful for EMTs to understand these interventions, and be prepared to support Paramedics in their application and use. This is why Advanced Life Saving (ALS) skills are covered as part of the EMT coursework. But not all calls require Paramedic interventions, and one the key takeaways I got from my time with Kathy and her partner Dave was just how critical the basic EMT assessment skills are in terms of determining when and why Paramedics are truly needed. After all, if they are responding to a call of questionable need simply because an EMT decided to request Paramedics "just in case", it certainly means that they are unavailable for someone else in a truly life-threatening situation.
0 Comments
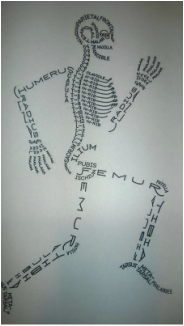
I had a conversation with one of our volunteers, Cliff, who is also taking EMT classes. As far as coursework goes, he's still in the beginning stages, learning basic anatomy and getting familiar with the steps of patient assessment.
As we're taught in class, patient assessment breaks down in to a series of discrete steps, starting with Scene Size-Up, moving in to a Primary Assessment for life-threats that require immediate interventions, and then on to Secondary Assessment and History Taking during which we more fully investigate the chief compliant(s) of our patients. Finally, we provide appropriate interventions and re-assessments while transporting them to the hospital. Cliff expressed concerns about the order of doing these various activities, ones that I also wrestled with. The coursework doesn't exactly feel right all the time, because the focus is on ensuring (and demonstrating) a complete understanding of ALL the steps in patient assessment, while the vast majority of real-world situations aren't nearly as linear. In particular, Cliff and I discussed the end step of the Primary Assessment (referred to as the "Transport Priority Decision"), and it really drove home for me the difference between reacting with a sense of urgency to an emergency situation, versus acting as if there is an emergency itself. My EMT course is being taught through Atlantic Training Center, using facilities at the Morris County Public Safety Academy. The Academy not only supports Police and Fire academies for the county, it's also co-located with the Morris County Office of Emergency Management (OEM) facilities. Although not formally part of the EMT course, my class was exceedingly lucky to have a quick tour of the 911 emergency dispatch center and the Emergency Operations Center (EOC), thanks to Scott DiGiralomo, Director, Department of Law and Public Safety/Emergency Management Coordinator. A mere 2 years old, the center is a technological marvel, reminiscent of any major Hollywood movie depicting high-tech command-and-control centers, from space flight operations to military war rooms. As my actual career has been in the high-tech and telecom industries for 25-plus years, I found the technical aspects quite fascinating, from real-time video feeds from around the county (including the helipad at Morristown Memorial Hospital, used by our county airborne paramedics), to GPS-enabled tracking of emergency services personnel and equipment.
The amazing job these emergency dispatchers perform really can't be understated. For those that are curious, I've linked to a YouTube video that gives you just a small taste of the complex multi-tasking these individuals perform, minute by minute, staying on-line with callers for as long as necessary with simultaneously coordinating with a host of dispatched resources. They truly are one of a kind, and probably don't get half the recognition that they deserve.
At this point in time, I'm almost to the midpoint of the EMT coursework. I've read almost 800 pages of the EMT book, and taken the online quizzes available to me so many times I'm probably mumbling "D, all of the above" in my sleep.
In class, we've been wrapping up materials related to medical emergencies, which cover all the major body systems, from cardiology to respiratory, endocrine to neurological. We've even touched on psychiatric emergencies, which may or may not have an associated underlying medical cause. and thus require us to keep an open mind when evaluating and caring for those in need. As an example, we ran an exercise in class where one student pretended to be both intoxicated and arrested, but in truth was suffering from impairment of their airway due to the position in which they were being held by police (and, of course, exacerbated by the effects of alcohol as well, which depressed their nervous system to the point of stupor). The goal of the exercises was to reinforce our responsibilities to ensuring the critical ABC's (airway, breathing, and circulation) remain viable, rather than allowing situational or prejudicial assumptions override our training. In this case, the presence of police and the expectations of a patient in an intoxicated state shouldn't have shifted the students focus from a patient exhibiting 'snoring respirations', which is a sign of airway compromise requiring immediate action to address. We're also covering gynecological emergencies in this section on medical emergencies, and it is because of the sensitive and personal nature of these issues that we are always seeking more women EMTs to join our squad. Well, actually... don't! There's no doubt that we've got to master the signs and symptoms, and associated interventions, of both respiratory and cardiac emergencies. Every situation we face starts with assessing the ABC"s -- Airway, Breathing, and Circulation -- as these represent true emergencies, where it really can be a matter of life-or-death.
Respiratory and cardiac emergencies are very closely related, as issues in one area can have a detrimental, even fatal, impact to the other.
While the heart is responsible for pumping blood through the lungs for oxygenation, and then moving the oxygenated blood itself to the tissues and organs throughout the body, it is itself a muscle that also requires oxygenated blood to effectively pump. So any disruption in how the body is obtaining and utilizing air through the upper and lower airways (including the lungs) can cause issues for the heart as well. And things roll downhill quickly from there on... Because having to perform CPR means that someone is having a really, really, really bad day.... With the first set of EMT written and practical tests behind us (Ashley, our Cadet member, and myself both scored very well...thanks to all who offered their well wishes!), our classwork moves on to a more focused set of lectures on medical emergencies, and their associated care and treatment options.
While we are told not to diagnose underlying causes of illness, in practice, EMTs play a very key role in uncovering critical signs and symptoms of those underlying medical issues through our history-taking activities (the aforementioned "million questions"), which we provide to medics and hospital staff as part of our transfer of patient care. The questions also guide us in developing an index of suspicion for what may be happening with our patient, allowing us to be more aware of the risks for cardiac, respiratory or neurological issues that may develop while we are in transport. Classwork this week focused on the various causes of respiratory distress. If you love to read a good detective story, this set of coursework is for you. The textbook almost reads like a good mystery novel, filled with similar signs and symptoms for many different potential causes of dyspnea (or shortness of breath). And only by combining the practical lung sound skills we're learning to listen for, with other vital signs (including pulse rate and blood pressure), key medical history, and signs and symptoms from our observations and the patients own behaviors and expressed issues, can we reach a clear index of suspicion on key underlying possibilities to be aware of. The first set of written and practical exams are coming up. I'm not as nervous as I thought I would be for the written portion, as there are a lot of resources available to EMT students in terms of online quizzes, eWorkbooks, and study aid apps for your favorite tablet or smartphone.
The practical portion of the exam is a bit more challenging, as it represents core skills that will be used over and over again, including patient assessment and vitals, airway management, plus lifting and moving skills. The upside, at least for me, is that my volunteering as a driver with the squad has given me a working understanding of much of this material, and so my focus is more on the mechanics of the process, making sure I don't miss or skip the specific order of actions, observations, or questions that I should be considering. The course instructors have been giving us specific drills to reinforce all these points, but it's still a lot of material to cover - almost 500 pages of the EMT book, plus lecture materials containing practical advice not explicitly found in the book or online lecture materials. Mostly, it's just a case of study, study, study.... Part of the practical skills we've been focusing on in class are the primary and secondary assessments that EMTs do on patients. While the primary assessment is done on scene, and focuses on managing life threats, the secondary assessment can be done on scene or in the back of the ambulance while we are transporting a patient to the appropriate medical center.
The secondary assessment, if we aren't still actively managing life threats (like performing CPR), allows for a more through inspection of the patient, either for a specific injury or illness symptom (assuming they are conscious and alert enough to talk with us), or a full-body scan intended to ensure we don't miss any additional injuries (which is especially important with an unconscious or unresponsive patient, or even a conscious one with an altered mental status). This also includes taking critical vital signs, including pulse and blood pressure, in order to determine if our interventions are producing the right positive results, or whether our patients are sliding towards dangerous grounds, such as shock. So ... Who would have thought that one of the best study aids I could get for this stuff would be my 8-year old son and his imagination? Well, not quite a million, perhaps. But a lot.
If you've ever had the need for an EMT's help, you've probably experienced the barrage of questions we ask. And we consider it a really good start when you're awake, alert, and able to answer those questions. Before our EMT classwork can start to talk about interventions for specific injuries or illnesses, it's important for us to identify what, exactly, we're dealing with. And while it's often easy to get the basics when you have a conscious and lucid patient, that isn't always the case. EMTs are drilled to take a specific step-by-step approach, called assessments, in order to ensure we first focus on critical life-threats, and then (and only then) identify and prioritize other issues our patients may be having. These assessments break down to the Primary Assessment (done when we first arrive on the scene), the Secondary Assessment (which may be done on scene, in the ambulance), and re-assessments as needed or warranted by the specific issues and interventions being undertaken. At this point in my EMT course work, we're starting to practice these assessment skills, linking signs and symptoms to the knowledge of anatomy we've been learning, before we move and transport patients anywhere else. And it comes with learning a bunch of mnemonics, such as AVPU, SAMPLE/OPQRST, and DCAP-BTLS (just to name a few), to ensure we don't miss any critical information.
The keys to providing effective care, however, requires us to understand human anatomy and how all the systems within our bodies both work and inter-relate. And while it is a major amount of stuff to learn, it's probably not much more than the average 8th grade health class or high school biology class.
|
AuthorJon Alperin, one of our MFAS volunteers, shares his journey to becoming an NJ certified EMT. from the Start
Here is Jon's journey, presented in time order:
Archives
June 2016
Categories
All
|



 RSS Feed
RSS Feed